Welcome to the Health & Rights Observatory. This platform has been designed and created by the Global Center for Health Diplomacy and Inclusion (CeHDI), to advance and amplify the mainstreaming of the right to health in the Human Rights Council processes, treaty bodies and special procedures as a gateway for universal health coverage and global health equity.
The Right to Health, as enshrined in Article 12 of the International Convenant on Economic, Social and Cultural Rights, is an inclusive human right that extends beyond timely and appropriate health care to encompass the underlying determinants of health. It forms an essential part of States’ obligations under international human rights law and provides a binding normative framework for advancing well-being, equity, and dignity across all sectors of society.
Under the Right to Health, States have the following obligations:
- Respect: refrain from directly or indirectly interfering with the enjoyment of the right to health.
- Protect: take effective measures to prevent third parties from undermining of violating the guarantees of the right to health.
- Fulfill: adopt appropriate legislative, administrative, budgetary, judicial, promotional, and other measures toward the full realization of the right to health.
The platform is intended to empower diplomats, policymakers, decision-makers across the health, foreign affairs, and related sectors, as well as civil society actors, to advance the Right to Health within global and national human rights discussions.
In the following pages, the platform presents data on the Right to Health within the context of the Universal Periodic Review (UPR). This State-led mechanism evaluates each state’s human rights obligations and commitments. The review process is participatory and includes interactive discussions during which any UN Member State may issue recommendations to the State under review, which may then choose to ‘support’ or ‘note’ those recommendations.
This platform us under active development, and we encourage you to contact the CeHDI team at info@cehdi.org for more information or to give feedback.
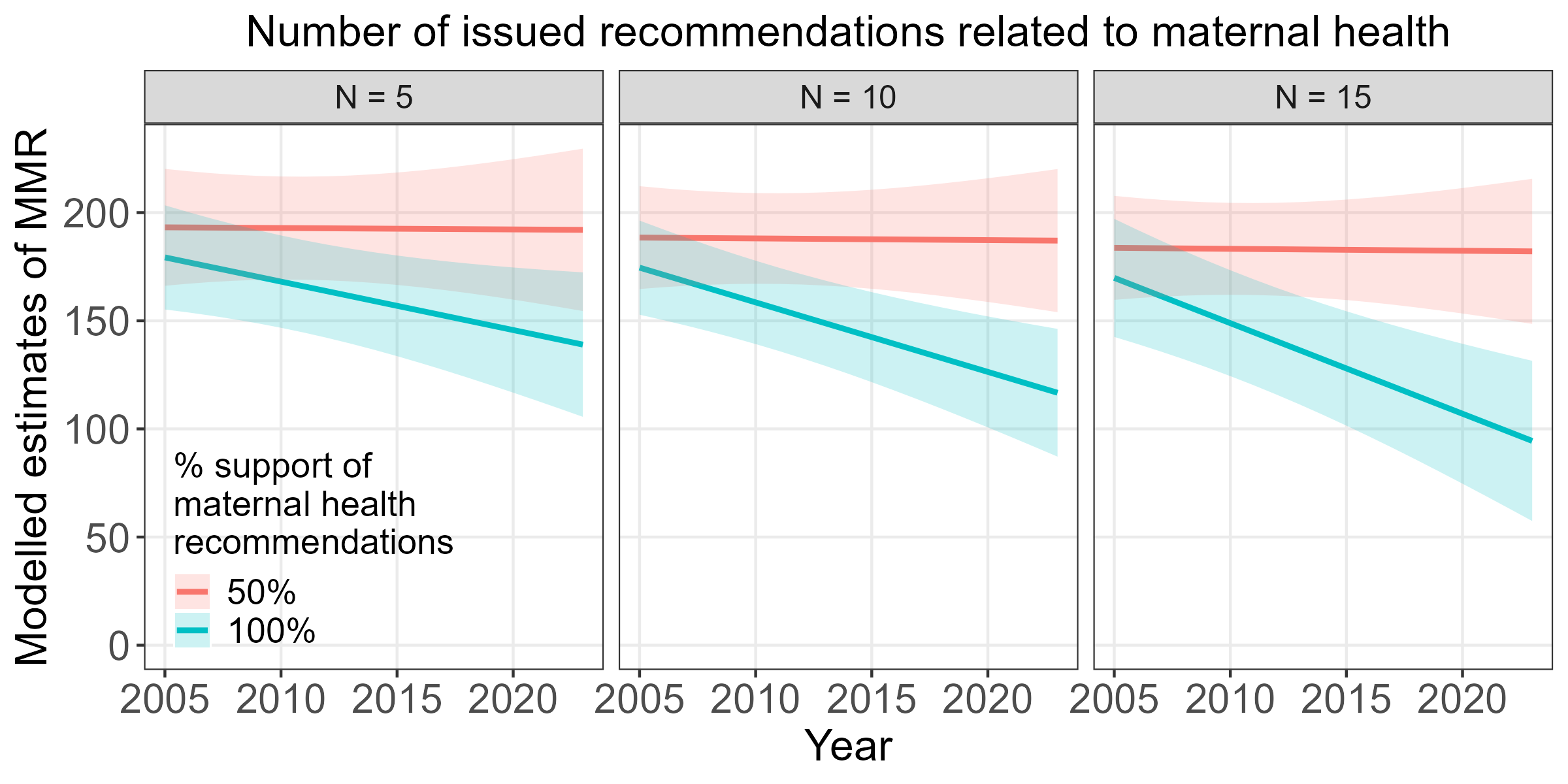
A preliminary analysis of recommendations related to maternal health suggests that higher engagement with the UPR process, in terms of the number of recommendations issued by reviewing states as well as support of recommendations by States Under Review, is associated with accelerated progress in reducing the maternal mortality ratio (MMR) over time.
UPR Recommendations by Region
UPR Recommendations by State
UHC: Universal Health Coverage
The below abbreviated definitions were compiled from the IHME's factsheets pages for the level 4 causes of maternal disorders:
Maternal haemorrhage includes both postpartum haemorrhage (defined as blood loss ≥500 ml for vaginal delivery and ≥1000 ml for caesarean delivery) and antepartum haemorrhage (defined as vaginal bleeding from any cause at or beyond 20 weeks of gestation).
Maternal sepsis is defined as a temperature <36°C or >38°C and clinical signs of shock (systolic blood pressure <90 mmHg and tachycardia >120 bpm). Other maternal infections are defined as any maternal infections excluding HIV, STI, or not related to pregnancy.
Maternal hypertensive disorders include gestational hypertension (onset after 20 weeks gestation), pre-eclampsia, severe preeclampsia, and eclampsia, but exclude chronic hypertension (onset prior to pregnancy or prior to 20 weeks gestation) unless superimposed preeclampsia or eclampsia develop.
Maternal obstructed labour and uterine rupture aggregates obstructed labour (arrest in the first or second stage of active labour despite sufficient contractions), uterine rupture (non-surgical breakdown of uterine wall), and fistula (an abnormal opening between the vagina and the bladder or rectum following childbirth).
Abortion is defined as elective or medically indicated termination of pregnancy at any gestational age. Miscarriage is defined as spontaneous loss of pregnancy before 24 weeks of gestation with complications requiring medical care.
Ectopic pregnancy is defined as pregnancy occurring outside of the uterus.
Indirect maternal deaths are due to existing diseases that are exacerbated by pregnancy. Examples include maternal infections and parasitic diseases complicating pregnancy, childbirth, and the puerperium, and diabetes in pregnancy, childbirth, and the puerperium.
Late maternal deaths are deaths that occur six weeks to one year after the end of pregnancy, excluding incidental deaths.
Maternal deaths aggravated by HIV/AIDS are deaths occurring in HIV-positive women whose pregnancy has exacerbated their HIV/AIDS, leading to death.
Other direct maternal disorders encompasses a wide range of maternal disorders that do not map to other diseases in the GBD cause list, including other fatal or non-fatal complications occurring during pregnancy, childbirth, and the postpartum period.