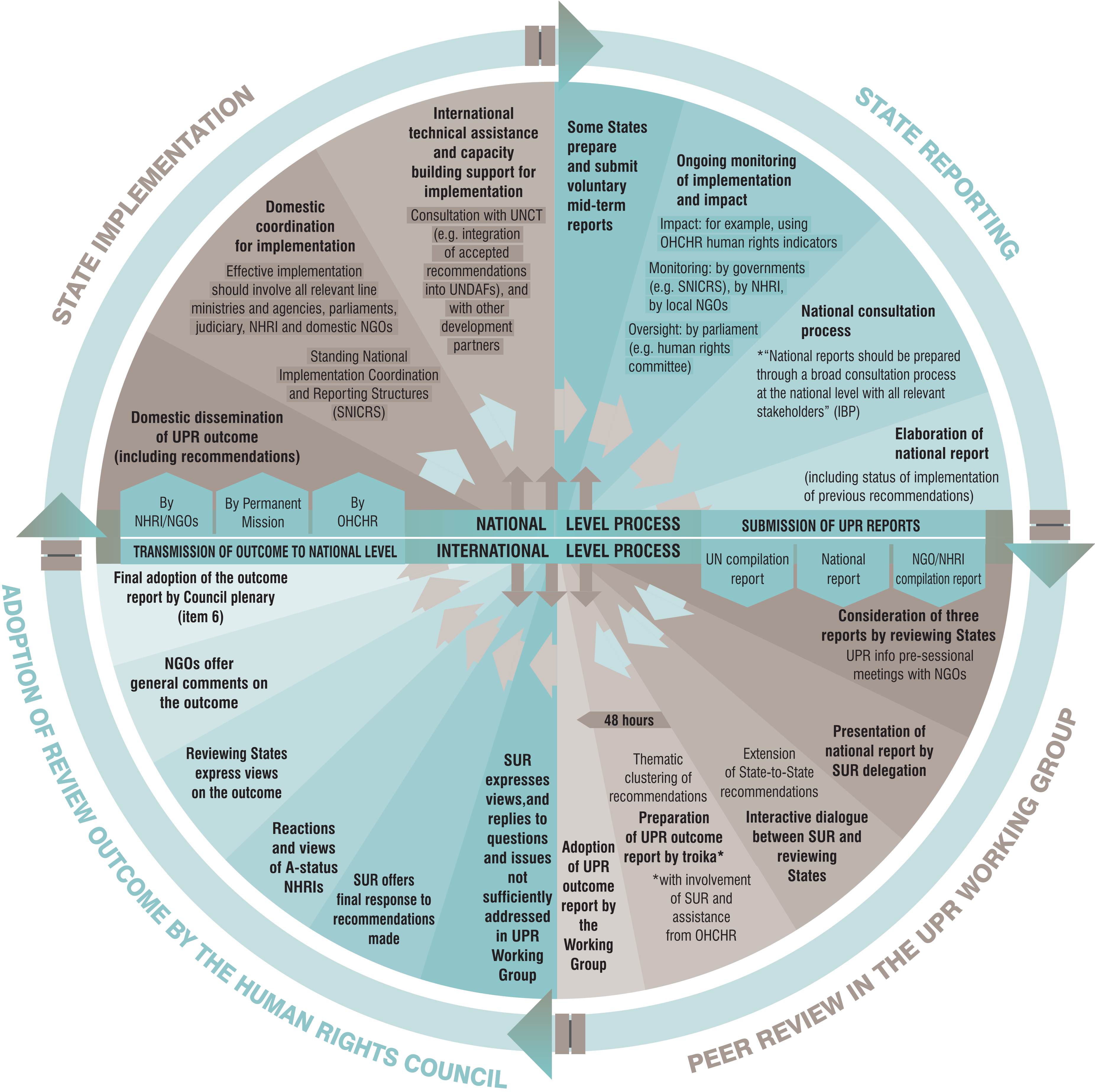
Welcome to the Health & Rights Observatory. This platform has been designed and created by the Global Center for Health Diplomacy and Inclusion (CeHDI), to advance and amplify the mainstreaming of the right to health in the Human Rights Council processes, treaty bodies and special procedures as a gateway for universal health coverage and global health equity. The platform is intended to empower diplomats and policymakers across the health, foreign affairs, and related sectors, as well as civil society actors, to advance the Right to Health within global and national human rights discussions.
The Right to Health, as enshrined in Article 12 of the International Convenant on Economic, Social and Cultural Rights, is an inclusive human right that extends beyond timely and appropriate health care to encompass the underlying determinants of health. It forms an essential part of States’ obligations under international human rights law and provides a binding normative framework for advancing well-being, equity, and dignity across all sectors of society.
Under the Right to Health, States have the following obligations:
- Respect: refrain from directly or indirectly interfering with the enjoyment of the right to health.
- Protect: take effective measures to prevent third parties from undermining or violating the guarantees of the right to health.
- Fulfill: adopt appropriate legislative, administrative, budgetary, judicial, promotional, and other measures toward the full realization of the right to health.
Click on a bar chart to view the text of the relevent UPR recommendations
Click on a bar chart to view the text of the relevent UPR recommendations
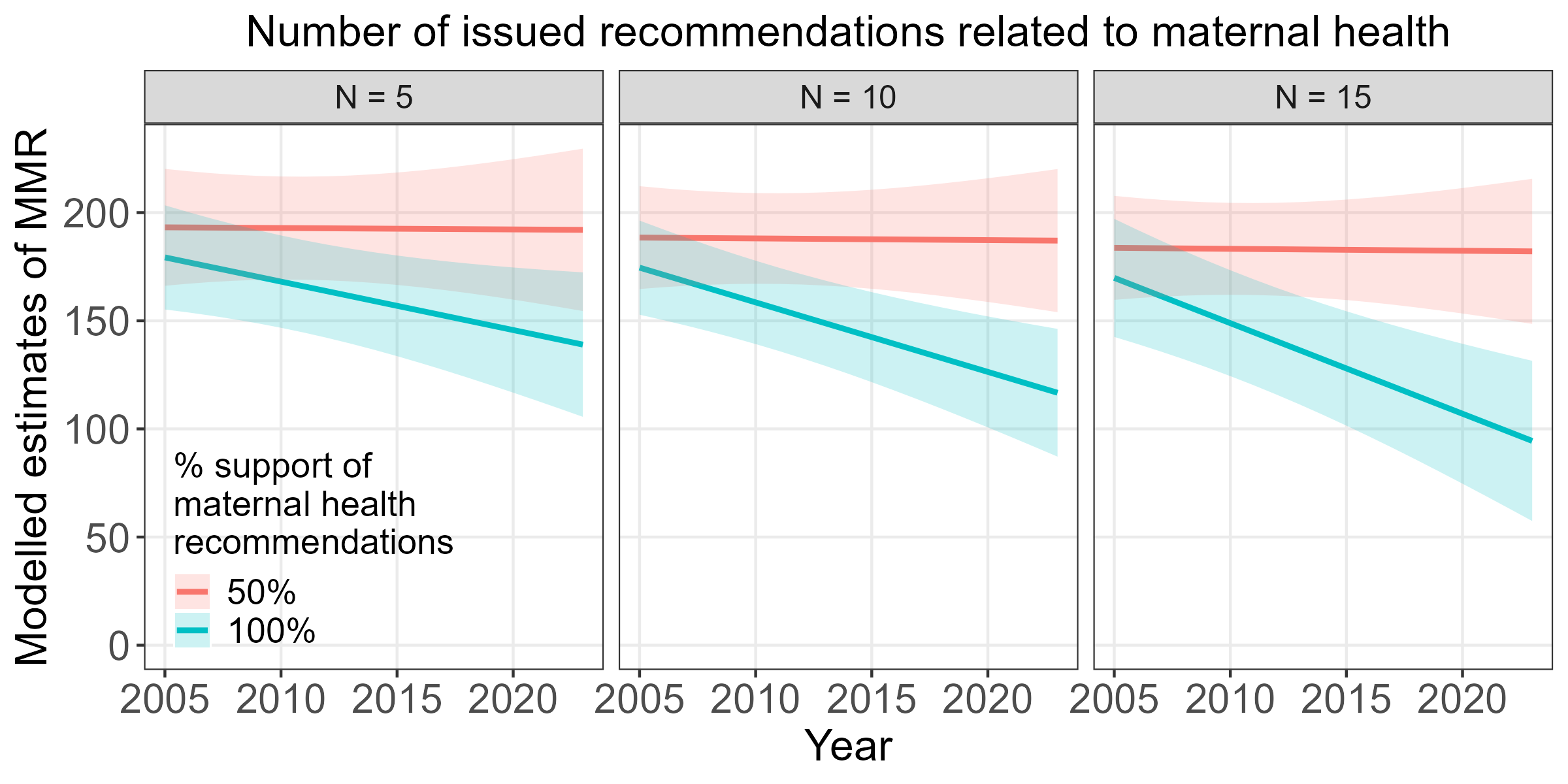
Maternal Mortality Ratio (MMR): Number of maternal deaths per 100,000 live births.
The below abbreviated definitions were compiled from the IHME's factsheets pages for the level 4 causes of maternal disorders:
Maternal haemorrhage includes both postpartum haemorrhage (defined as blood loss ≥500 ml for vaginal delivery and ≥1000 ml for caesarean delivery) and antepartum haemorrhage (defined as vaginal bleeding from any cause at or beyond 20 weeks of gestation).
Maternal sepsis is defined as a temperature <36°C or >38°C and clinical signs of shock (systolic blood pressure <90 mmHg and tachycardia >120 bpm). Other maternal infections are defined as any maternal infections excluding HIV, STI, or not related to pregnancy.
Maternal hypertensive disorders include gestational hypertension (onset after 20 weeks gestation), pre-eclampsia, severe preeclampsia, and eclampsia, but exclude chronic hypertension (onset prior to pregnancy or prior to 20 weeks gestation) unless superimposed preeclampsia or eclampsia develop.
Maternal obstructed labour and uterine rupture aggregates obstructed labour (arrest in the first or second stage of active labour despite sufficient contractions), uterine rupture (non-surgical breakdown of uterine wall), and fistula (an abnormal opening between the vagina and the bladder or rectum following childbirth).
Abortion is defined as elective or medically indicated termination of pregnancy at any gestational age. Miscarriage is defined as spontaneous loss of pregnancy before 24 weeks of gestation with complications requiring medical care.
Ectopic pregnancy is defined as pregnancy occurring outside of the uterus.
Indirect maternal deaths are due to existing diseases that are exacerbated by pregnancy. Examples include maternal infections and parasitic diseases complicating pregnancy, childbirth, and the puerperium, and diabetes in pregnancy, childbirth, and the puerperium.
Late maternal deaths are deaths that occur six weeks to one year after the end of pregnancy, excluding incidental deaths.
Maternal deaths aggravated by HIV/AIDS are deaths occurring in HIV-positive women whose pregnancy has exacerbated their HIV/AIDS, leading to death.
Other direct maternal disorders encompasses a wide range of maternal disorders that do not map to other diseases in the GBD cause list, including other fatal or non-fatal complications occurring during pregnancy, childbirth, and the postpartum period.
Women of reproductive age (aged 15-49 years) who have their need for family planning satisfied with modern methods (%). Data: WHO
Approaches to health include the right to health, public health, or medical care. Data: World Policy Center